Yesterday’s post has stimulated a lot of interesting discussion on Twitter. I have updated the post with some of the tweets. Here are two more that have stimulated some additional thoughts:
@kidney_boy In a case like this would dialysis be better? Or if youre just going to give him free water back, what about a loop diuretic too?
— Matthew Wong (@MatthewLWong) June 11, 2013
@kidney_boy @skepticscalpel This and water poker poisoning incident. Posters for “the dose makes the poison.”
— Casey Lyons (@lyonscas) June 10, 2013
When I was discussing the case with my dad, a surgeon, he kept asking if I would have given a diuretic. I wouldn’t. In fact I wouldn’t have managed the case like the doctors in the case report did.
Now before I express my criticism, it must be noted that the doctors took on a lethal poisoning and undoubtedly saved his life. Criticizing their management may appear to be deducting style points from a walk off home run, who cares if they swung at a bad pitch, they won the game. I want to recognize the bravery, intelligence and success of the medical team but I don’t think it was ideal care and I feel they were just as lucky as they were good.
The crux of their treatment was a massive infusion of D5W. Dextrose infusions are the bedrock of treatment of hypernatremia. The reason is that most routine cases of hypernatremia are due to water deficits:
- diabetes insipidis
- dehydration
- altered mental status
- disrupted thirst mechanics.
Outside of treating the side effects of too much sodium bicarbonate (remember the sodium concentration in an amp of sodium bicarbonate is 1,000 mmol/L) we don’t routinely see hypernatremia from salt overdoses.
This patient did not suffer a water deficit, he had salt overdose, a month worth of sodium in a single quart. I think the infusion of 6 liters of D5W in 30 minutes had a high chance of causing serious problems, especially since the patient in question was not volume or water depleted. Not only was he not volume depleted, the high serum sodium was pulling water from the intracellular compartment and shifting it to the interstitial and vascular space, so not only was he not volume depleted, he likely was volume expanded. The treating doctors took a patient with a lethal sodium ingestion and treated it with a lethal water ingestion (Jennifer Strange who died in the tragic Wee for a Wii incident ingested 7.5 liters over 2 hours).

While in most cases of hypernatremia we give water because that is what is missing, in this case we need to remove the sodium. The treating doctors decided to depend on the kidneys to clear the excess sodium. The kidneys did an admirable job with extremely high urine sodium levels and concentrated urine, however they made that decision while his creatinine was going up. That seems a bit questionable.
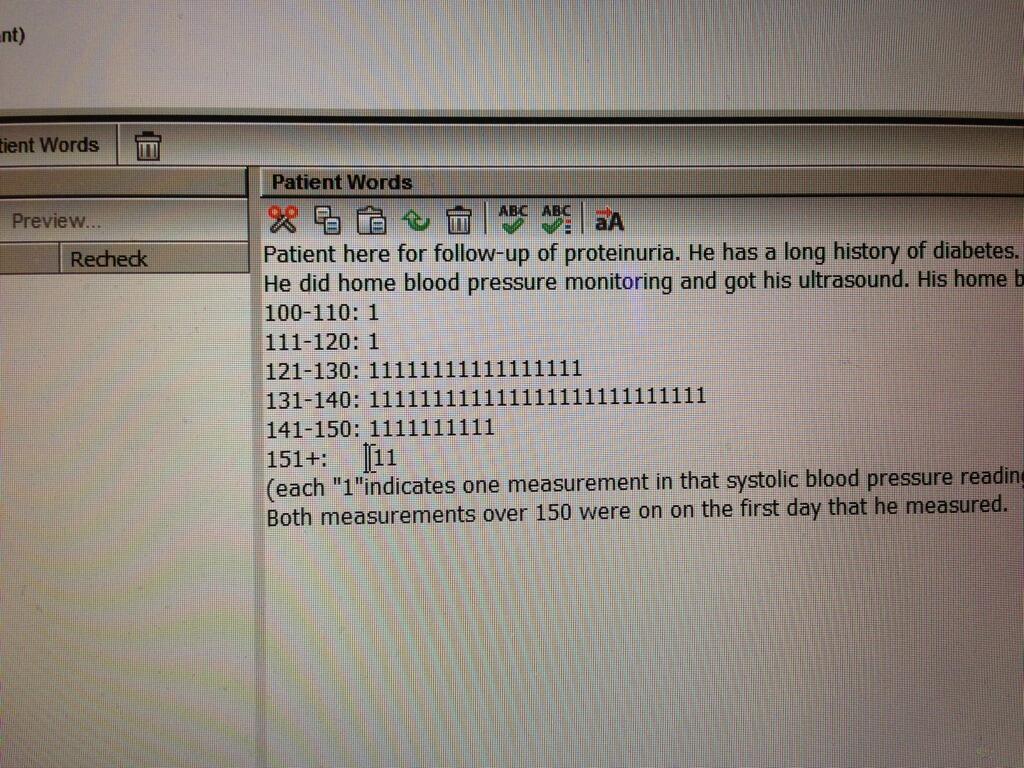
The fluid also raised his glucose and lowered his potassium (the D5W infusion dropped the potassium from 5.1 to 2.5 in 30 minutes, I suspect this was an insulin effect). The increased glucose actually blunted the decrease in osmolality that occurred during treatment. In fact if you calculate the osmolality, the infusion of D5W had a surprisingly modest effect on serum osmolality, especially compared to it’s effect on the sodium concentration.
 |
| If you do any math on your Mac you stop using the calculator and buy Soulver. |
 |
| Large change in sodium with 6 liter D5W infusion |
 |
| Much more modest change in osmolality due to D5W induced hyperglycemia |
Again, the treatment worked and perhaps the hyperglycemia helped protect the brain or ameliorated the cerebral desiccation of hypernatremia. I don’t know.
Some may argue that since glucose is not an effective osmole we should not be concerned about it. I think it was an effective osmole do to the lack of insulin activity (evidenced by the high serum glucose). Just like we see cerebral edema from the rapid reduction of glucose in kids being treated for DKA, that is a situation where changes in a normally ineffective osmole cause movement of water.
My dad wanted to use a diuretic because he wanted to get rid of the ingested sodium as fast as possible. The problem with a diuretic is it will decrease the maximum urine concentration so that sodium excretion occurs at a lower urine osmolality increasing urinary water losses, exactly what you don’t want in this situation. The patient was making a large amount of urine and eventually got his urine sodium up to 270 mmol/L and urine osmolality up to nearly 1,000 mOsm/Kg H2O. If he was given furosemide he would not have been able to achieve that degree of efficiency.
I would have been nervous about trying to administer 6 liters of fluid in 30 minutes and assuming dialysis could be arranged to run without delay (impossible in the middle of the night and difficult to assure during the day) I would have selected that option. The reason I like dialysis is that it would remove the toxin, sodium.
Something that most non-nephrologists don’t recognize about dialysis is that though hemodialysis removes sodium it does not remove it by diffusion, the process by which it removes every other toxin. The dialysate has a sodium concentration that runs from 140 to 150 mmol/L, essentially isotonic. No concentration gradient means no clearance from diffusion. Sodium is removed by ultrafiltration. That means when we remove 4 liters of fluid with dialysis (we essentially use the pumps to squeeze 4 liters of plasma through the membrane’s pores, and those four liters contain isotonic sodium, so 4 liters x 140 mmol/L = 560 mmol of sodium removed from the body.

In this situation there would some removal of sodium by diffusion because of the extreme hypernatremia and there would be additional removal by ultrafiltration, depending on how much fluid I removed. I would start a D5W infusion at a liter an hour and remove 4 liters of fluid over a four hour treatment. I would check plasma sodium and osmolality every hour and, and, I don’t know how fast I would go:
- Should I try to normalize the sodium as fast as possible?
- Should I lower the sodium as fast as possible until the seizing stops and spontaneous movement returns?
- Should I lower the sodium at a target rate of 12 mmol/L per hour? 5 mmol/L per hour? 2 mmol/L per hour?
I don’t know but if forced to make a decision I think I would go with answer 2.
How would you manage a sodium of 191?