I received this tweet a few days ago:
.@pbjpaulito Did you know about this? http://t.co/ttcnT21GCzcc @kidney_boy
— Meenakshi Budhraja (@gastromom) June 29, 2013
The link goes to this article at the Huffington Post Journal of Medicine and this article from 2012:
The story is about a mystery epidemic causing widespread chronic kidney disease and end-stage renal disease in the farmers of Central America. Here is a less sensational view of the epidemic. The best part of the article is the five paragraphs that quote three independent experts that all agree that the most likely etiology is repeated episodes of dehydration:
“I think that everything points away from pesticides,” said Dr. Catharina Wesseling, an occupational and environmental epidemiologist who also is regional director of the Program on Work, Health and Environment in Central America. “It is too multinational; it is too spread out.
“I would place my bet on repeated dehydration, acute attacks everyday. That is my bet, my guess, but nothing is proved.”
Dr. Richard J. Johnson*, a kidney specialist at the University of Colorado, Denver, is working with other researchers investigating the cause of the disease. They too suspect chronic dehydration. “This is a new concept, but there’s some evidence supporting it,” Johnson said. “There are other ways to damage the kidney. Heavy metals, chemicals, toxins have all been considered, but to date there have been no leading candidates to explain what’s going on in Nicaragua… As these possibilities get exhausted, recurrent dehydration is moving up on the list.”
This reasoned diatribe is followed by this:
…scientists have no doubt they are facing something deadly and previously unknown to medicine.
Did the authors even read their own article? Dehydration would hardly be something unknown to medicine. After that, the article really goes off the rails with statements like:
In nations with more developed health systems, the disease that impairs the kidney’s ability to cleanse the blood is diagnosed relatively early and treated with dialysis in medical clinics. In Central America, many of the victims treat themselves at home with a cheaper but less efficient form of dialysis, or go without any dialysis at all.
Newsflash: peritoneal dialysis (the cheaper dialysis that you do at home), is not less efficient than hemodialysis.
The article tips an article that was to be published soon:
Some 30 percent of coastal dwellers had elevated levels of creatinine, strongly suggesting environment rather than agrochemicals was to blame, Brooks, the epidemiologist, said. The study is expected to be published in a peer-reviewed journal in coming weeks.
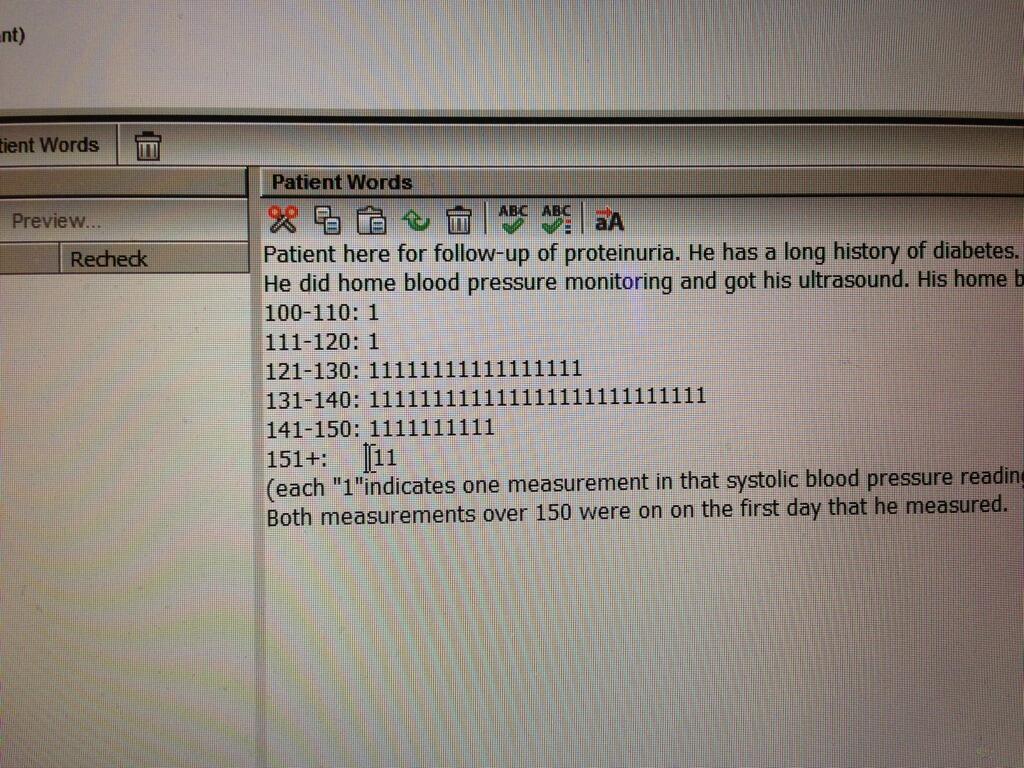
That article is now available. Here is the primary figure of the article:
 |
| masl is meters above sea level |
The finding that high altitude is protective is not new, but this study was the first to show it in El Salvador. That is importnat because in El Salvador, sugar cane is harvested at both low altitude and high altitude, so previous findings had been confounded by different crops at the two altitudes.
Also they did some nice work showing a dose response:
It is an interesting story and I am going to keep my ear perked for more information.
Some facts about this CKD epidemic:
- Men outnumber women 3:1
- diagnosis typically is in the fourth decade of life
- Proteinuria is uncommon
- biopsies have been infrequently done but when available show a tubulointerstitial process with small fibrotic kidneys
- industries that have high prevalence of disease are:
- sugarcane cultivation
- mining
- fishing
- shipping
- Industries with low prevalence
- coffee growing
- service sector
- low altitude has a higher risk than high altitude