Gr8 quest! Lets ask @kidney_boy @deanoburns “When following UO in morbidly obese&using 0.5ml/kg/hr do U use actual,ideal or adjusted weight?
— Haney Mallemat (@CriticalCareNow) August 29, 2013
The short answer is just use the patients mass. No need for ideal or adjusted weight.
The long answer follows: To answer this I’m gonna to proceed from first principles. Why do we measure urine output? It is the most fundamental and basic measures of renal function. Before there were MDRD, creatinine or a Chem-7 we could measure the urine output. A biochemical urinalysis meant tasting it.
Oliguria means the urine output has fallen below the minimal healthy amount. (NEJM Review) So how much urine do people need to make to stay healthy? The flippant answer is enough, enough for what? Enough to stay in balance. Enough that every drop of water that is ingested is then excreted. Enough that every microgram of solute is excreted.
In regards to water, some will be lost with respiration, some in stool and some through the skin, but whatever is left over must be excreted by the kidneys. If water is not excreted and accumulates patients develop hyponatremia.
In regards to solute, proteins, electrolytes and minerals are constantly being absorbed by our indiscriminate digestive tracks. All of them most be accounted for and must either be incorporated into the body (growth) or cleared out, most of this work devolves on the kidney. If solute is not excreted it will accumulate and we will see increases in BUN from protein, edema from salt accumulation and other symptoms from the infinite variety of solutes we take in.
Obviously, accumulation of solutes is the factor whose symptoms better correlate with out definition of renal failure, so oliguria should be defined as the urine output, below which, people begin to accumulate solute. This volume is highly dependent on the diet. If the patient is eating a tiny amount of solute they will be able to have a very low urine output without beginning to accumulate solutes.
But the definition of oliguria is not built for these edge cases, it is designed to answer the question, what is the minimum amount of urine a person could make and still get rid of all the solute of a regular diet.
This math is pretty straight forward:
The definition of oliguria is 400 or 500 mL per day. The 583 on a normal diet is pretty close. If acutely ill patients decrease solute intake their minimal urine volume will creep down to the established 400-500 mL limits.
But this sets up the question, “Does urine output matter? Is it superior to biochemical assessments of renal function? Does the fact that I can order a serum creatinine every 12 hours make following hourly urine output unimportant?”
The answer is No. Urine output provides additional information on renal function that can not be seen with serum creatinine. Urine output increases the sensitivity of the RIFLE and AKIN definitions of AKI without compromising specificity. Increased sensitivity means that when combing through a cohort of patients, the addition of urine output will roughly double the number of patients flagged with AKI. Maintaining specificity means that clinical outcomes of these patients will be roughly identical to patients who meet AKI criteria due to changes in creatinine.
Sensitivity data: the use of oliguria roughly doubled the incidence of AKI from 24 to 52% of this cohort. While specificity was maintained:
In this multi-center, prospective study, however, they found differing conclusions. Though oliguria was associated with AKI from Cr, the relationship was to lose to be clinically useful. Oliguria was frequent, they found it in one third of ICU days. This resulted is a high false positive rate of AKI. They also found that half of patients who develop AKI by creatinine did not have oliguria for 4 or more hours the day prior and a quarter did not have oliguria at all. Only when they increased the duration of oliguria to at least 12 hours did the likelihood ratio rise above 10 (necessary for a clinically useful test) but this dramatically dropped the specificity of oliguria to the point that it would miss over half the cases of AKI.
So the addition of oliguria does add sensitivity without additional loss of specificity but in no way can oliguria displace creatinine as a reliable and early detector of AKI.
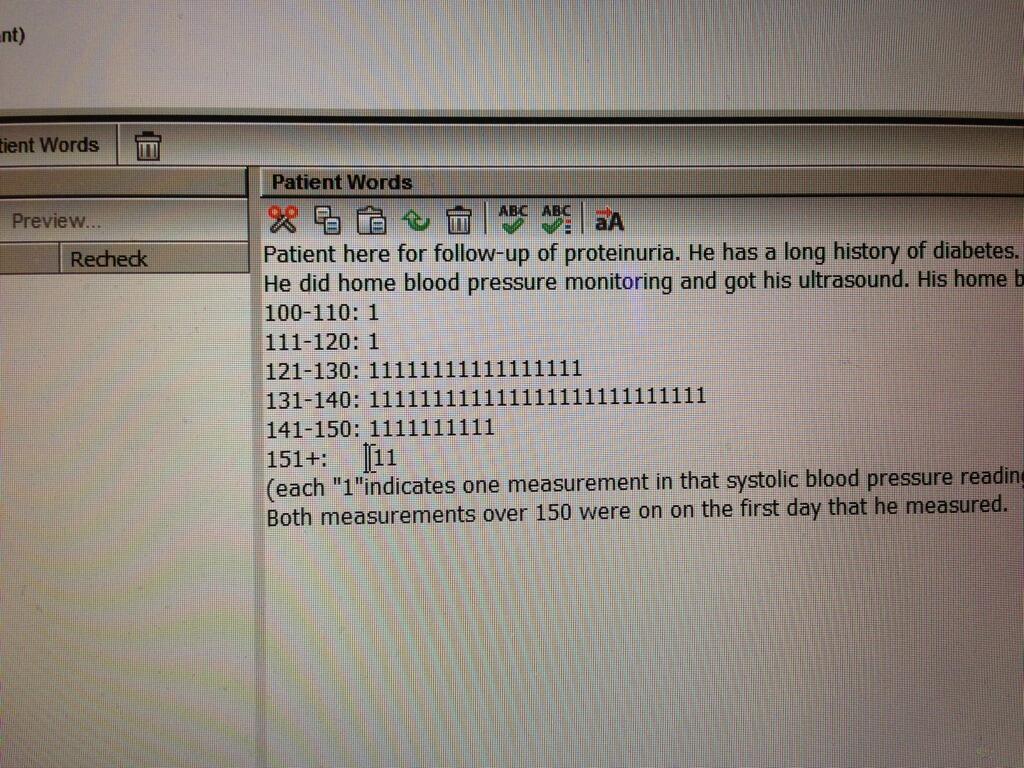
Looking through the data collected on using urine output to define AKI and predict outcome, they do not use ideal weight or adjusted weight, just straight mass. It would be interesting for someone to re-run the analysis on the previously collected data using ideal or adjusted weight and see if oliguria became a better biomarker of acute kidney injury.
What a crappy text book, it doesn’t even have “oilguria” in it. Who wrote this piece of…? oh. pic.twitter.com/U1JRBLji89
— Joel Topf (@kidney_boy) September 6, 2013