Nephrology Education Legends
There are a few legendary nephrology education experiences:
- The Brigham’s Board Review Class
- Renal Pathology at Columbia
- ASN Board Review (classically in San Francisco, but now ensconced in Chicago)
- University of Colorado Electrolyte Review in Aspen
Third signature
Bayesian statistics and the absurdity of 70% sensitivity for colon cancer
I saw a patient with this lab in their chart:
Who the hell thought a test with a sensitivity of 70% would make a good screening test? pic.twitter.com/PvO21omMFJ— Joel Topf, MD FACP (@kidney_boy) March 30, 2016
@kidney_boy sens+spec impt in diagnostics, also I think you’re missing that test is for those who can’t/won’t be screened by other methods— Shannon P (@kentuckyshan) March 30, 2016
I don’t know anything about Methylated Septin and not much more about colon cancer but a 70% sensitivity for a screening test seems a bit absurd. So I ran the numbers.
Using a colon cancer prevalence of 1,169,000 in the U.S. compared to an adult population of 245,270,000 gives a pre-test probability of 0.47%.
Getting a negative Methylated Septin result lowers the post-test probability to 0.2%.
Getting a positive Methylated Septin result increases the post-test probability to 2.9%.
Think about that, 97% of the people with a positive Methylated Septin* are actually cancer free.
*assuming you are testing an unselected population.
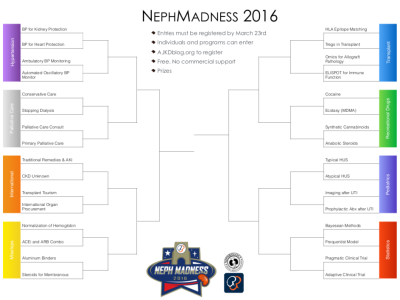
The essential lesson from the Missteps in Nephrology #NephMadness Bracket
The idea of a bracket full of nephrology mistakes was a bit controversial. Matt and I are pretty optimistic about the field of nephrology and really want NephMadness to showcase the best of the specialty. So how can a bracket of missteps fit into that idea?
The vision was to explore the moments nephrology went off the rails in order to inoculate us from making the same mistake in the future. Its okay to make mistakes, as long as we don’t keep making the same mistakes. The four missteps we chose each demonstrate a unique failure.
In chronologic order lets review the nature of the missteps.
Aluminum
Science is hard
A generation of patients suffered CNS, bone, and blood pathology from aluminum hydroxide prescribed to patients in order to prevent hyperphosphatemia. This was the young science of dialysis coming up against the limits of technology. Sure, there was the assumption that oral aluminum could not be absorbed, that was later shown to be false, but in the end, science is hard and mistakes are made when we are operating at the event horizon of knowledge. The lesson here should be that we should remain humble and maintain an open mind when operating at the edge of science. Long held assumptions can turn out to be wrong and harm can come from the most banal of sources. A phos binder. Really?
Steroids for Membranous
Statistics are a bitch
The positive finding in the Collaborative Study of Adult Nephrotic Syndrome is a cruel twist of fate. When examining the Missteps, I wanted to find a villain in each story I wanted each one to be a modern medical morality tale. I looked for a way to blame the greedy, or the arrogant, or the sloppy, but the story of membranous is just a story about bad luck affecting good people trying their hardest to do honest science. Dumb luck resulted in 9 of the most aggressive cases of membranous nephropathy all landing in the placebo group. The steroids didn’t preserve function, the placebo group just crashed and burned for no good reason. Bad things happen to good science. It happens because statistics demands it. Our only defense is to be vigilant against over interpreting fragile results and single trials.
Duel ACEi and ARB for Proteinuric Chronic Kidney Disease
It is easiest to fool people who want to believe
The story of of combining of ACEi and ARB is the classic medical reversal. The physiology and pathology tells explain that proteinuria is toxic. Two drug classes ACEi and ARBs have each separately been shown to be safe, effective and kidney protective. Early data shows that combining them unlocks synergistic reductions in the consensus surrogate outcome, proteinuria. The story was only missing improved hard outcomes with ACEi ARB therapy. This was satisfied by the 2002 COOPERATE trial in the Lancet. The trial answered all the hopes and dreams of nephrologists. It showed successful retardation of proteinuria and delayed dialysis. But when the trial is everything you ever hoped for, it probably would be wise to take a second look and go through the results patient by patient. The COOPERATE trial turned out to be a fraud. What is the lesson from ACEi and ARB? Stories that fit together like a perfect little present probably don’t and deserve special scrutiny.
Normalization of Hemoglobin
Don’t be distracted by the perfect little story, keep your eyes on the prospective data
Medical marketing used to mean mugs, pens and ads in journals. Now it means thought leaders, surrogate outcomes, studies and guidelines.— Joel Topf, MD FACP (@kidney_boy) March 31, 2016
Great #NephMadness infographic from NSMC intern Silvi Shah
Dr. Shah showed me how to make an infographic. Here’s her chart talking about Transplant tourism for NephMadness:
I then tried my hand at PiktoChart. Here’s mine:
Pediatricization of Nephrology
I did a Med-Peds residency. Very early in residency I knew that I did not want to do general pediatrics. I saw the field as largely being a caretaker of normal growth and maturation for the vast majority of patients (can we call them patients if they do not have a medical condition?) while at the same time being supremely vigilant to find the one in a thousand kids whose fever was not otitis media or adenovirus but bacterial meningitis. Primary pediatricians were ridiculed by the house staff for being over vigilant and admitting every cough, fever and rash or being idiots for missing obvious severe illness. From my eyes it looked like a horrible job.
Fast forward two decades and I find the overwhelming majority of new consults being for CKD stage 3 that after a thorough work-up ends up being normal renal deterioration of aging. I am becoming a caretaker of normal aging and maturation. Instead of trying to pick out the bacterial meningitis from a collection of fevers, I am trying to find the GN in a seas of decreased renal functions and diabetic kidney disease.
And like pediatrics, more and more of my job is spent reassuring people that the decreased renal function on their labs is not going to mean that they will be on dialysis. My most overused metaphor:
Just because you aren’t as fast a runner as you were when you were 22, doesn’t mean that you will end up in a wheel chair.
I know Go and Levey tell me that the decreased renal function is associated with increased risk of death, but no one can then offer me any evidence-based interventions to affect that risk. As long as it is impossible for me to intervene I am unable to shake the conclusion that this loss of renal function is natural aging.
This is the unintended consequence of the CKD staging system. We have fetishized GFR over pathology.
Kidney Stone lecture version 1.0
This lecture is treatment and practical focused lecture. Intended audience is nephrology nurse practitioners.
Based on the AUA stone guidelines (PDF), which are excellent.
Kidney Stones – Created with Haiku Deck, presentation software that inspires
Link to an Excel Spreadsheet of Oxalate content from various foods that is referenced in the AUA guideline. 657 rows!.
#HPM Chat Wednesday March 23 at 9PM Eastern: #NephMadness and the Palliative Care Region
Last year I hosted a Hospice and Palliative Medicine chat. That chat focused on Tamura’s ground breaking study, Functional Status of Elderly Adults before and after Initiation of Dialysis. Take a look at the blog post introducing that chat:
Have you ever read a journal article and as soon as you finished the abstract you had this forbidding feeling that if the authors actually proved what they claimed to have discovered your medical life will never be the same?
This happened to me when I read, “Functional Status of Elderly Adults before and after Initiation of Dialysis (OPEN ACCESS)” by Tamura et al. in 2009.
In that post I wrote, “While this study did not track patients who deferred dialysis it is hard to imagine they could do much worse.” Well just last month, the other shoe dropped. We now have a well executed study that does look at the patients who deferred dialysis for conservative care:
 |
| PDF version for your Trapper Keeper |
- Conservative care
- Stopping Dialysis
- Palliative Care Consult
- Primary Palliative care














