Abacavir and methanol poisoning
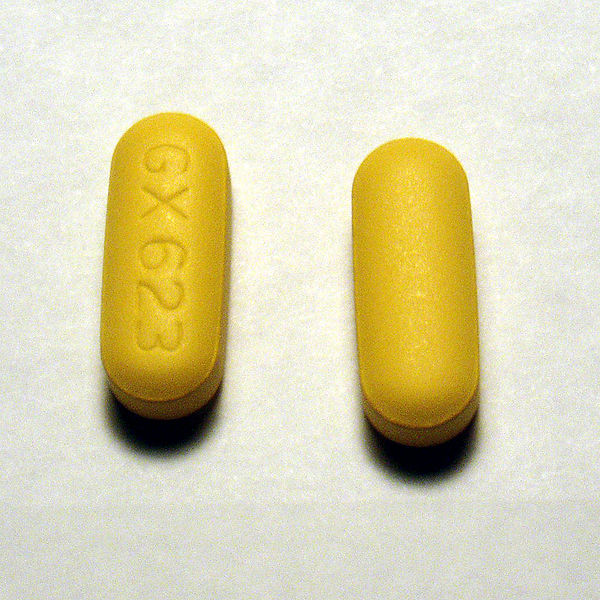
About a month ago, Nephron Power wrote about a great electrolyte case in AJKD. The case regarded a patient who drank a liter of methanol but was asymptomatic. The reason the patient was apparently resistant to a toxic methanol slug of methanol (The quantity of methanol that produces toxicity ranges from 15 to 500 ml of a 40% solution to 60 to 600 ml of pure methanol) was protective powers of abacavir. Abacavir is a nucleoside reverse transcriptase inhibitor and apparently, is a potant inhibitor of alcohol dehydrogenase, the critical enzyme which converts methanol into formaldehyde. Formaldehyde is then converted into the lethal formic acid by formaldehyde dehydrogenase.
After reading this I started to wonder if abacavir was such an effective inhibitor of alcohol dehydrogenase what happens when patients get exposed to say a more common substrate of alcohol dehydrogenase such as whiskey. Shouldn’t we hear about people on abacavir going on alcohol benders after a single shot of ethanol?
A couple of cracks at PubMed and I sure didn’t find much. Barber, Marrett et al. looked for two types of alcohol reactions from abacavir, either a disulfaram-like reaction or reduced alcohol tolerance. The authors found three cases of in 173 patients starting abacavir. They found one disulfarem reaction (nausea, tachycardia, flushing with a single shock of vodka) and two cases of decreased alcohol tolerance
After three glasses of wine he felt as though he had a bottle and a half, with memory loss.
The only other paper I could find was by McDowell, Chittick, et al. who looked at increased abacavir levels with alcohol intake. The reverse of what I was looking for, but at least it was related. They gave a single dose of abacavir and 0.7 g/kg of ethyl alcohol to 25 HIV positive men. They found a 26% increase in the half life of abacavir with alcohol but…
This study did not demonstrate any alteration in the pharmacokinetic parameters of ethanol by abacavir coadministration; blood ethanol median profiles following ethanol administration in the presence and absence of abacavir were essentially superimposable. There was no evidence that co-administration of abacavir interferes with ethanol metabolism. There were no disulfiram-type reactions in any subject who received coadministration of abacavir and ethanol.
This study tested the effects of a single dose of abacavir, chronic dosing may result in a different effect on alcohol dehydrogenase.
Interesting case nonetheless.
Flattering review of the Fluid and Electrolyte Companion
Not everyday that you get a new review of a ten year old book. Thanks Beaver Medic.
My feelings about kidney transplant
David Spiegel on the treatment of dialysis patients
There are only two outcomes that are important: quantity of life and quality of life. We don’t know how to measure quality of life and haven’t shown an ability to change the former.
– Posted using BlogPress from my iPad
The dangers of high dose vitamin D
Back in November I posted on a patient who had a dramatic improvement in her PTH following correction of her vitamin D deficiency. One of the comments was:
Anonymous said…
Why wait one entire year to correct the Deficiency. I would have treated with 100,000 units po qd for 5-10 days.I responded…
Regarding the time to treat the patient. This patient had almost no appreciable renal disease outside of the SHPTH. I was not going to schedule frequent visits to monitor therapy I just put them on a safe and familiar vitamin D dose and followed up every six months. I don’t think I harmed the patient with slow therapy. The one time I had a patient on 50,000 units daily (resident error) they were readmitted within 2 weeks with hypercalcemia.
The sugar in soda
From a pretty good article in Fast Company of all places:
But come on, are sodas really so bad? Even coffee drinkers like to use a little sugar. Should we demonize coffee, too? Well, as a thought experiment, imagine that you’re in the office kitchen as a colleague adds some sugar to his coffee. As you watch, he adds a teaspoon. And then another. And another. And another. And another. And another. And another.And another. And another. And another. And another. And another. And another. And another. And another. And another. (Dude, want some coffee with your sugar?)
Hyperkalemia as an indication for dialysis
A few weeks ago we admitted a patient who has been approaching ESRD for a number of years. Most of her medical care had been provided in the hospital as she bounced from admission to admission. Though we tried to get her into our CKD clinic she always failed to show up. You can track the progression of her CKD from hospitalization to hospitalization with a gradually increasing baseline creatinine.
On this most recent admission, she came in with the triple 8s:
- Hemoglobin 8.8
- Creatinine 8.1
- Potassium 8.6
Here is her initial EKG with that potassium:
The likelihood of renal replacement therapy, either transplant or dialysis, was near zero (≤1.3%) for patients in all stages except stage 4, where 2.3% ± 1.1% of patients received a transplant and 17.6% ± 2.7% had dialysis initiated.
iGot an iPad
I got a 3g model on Friday and I’m still trying to figure out what I’m going to use it for. How/if am I going to incorporate it into teaching.

In a large series of 382 patients with serum CK concentration >5000 U/L, 154 (40 percent) were treated with bicarbonate and mannitol [33]. There was no statistically significant difference in the incidence of renal failure (creatinine >2.0 mg/dL [177 micromol/L]; 22 versus 18 percent), dialysis (7 versus 6 percent), or death (15 versus 18 percent) in patients who were or were not treated with bicarbonate and mannitol. However, there was a trend toward improved outcomes in patients with extremely high CK levels (>30,000 U/L) treated with bicarbonate and mannitol.
Reference 33 is the primary reference for one of my first blog posts. We started talking about this study on rounds, but the crap machines in the ICU didn’t have Flash or PDF support. I ended up downloading the PDF on my iPhone and four of us passed it around to look at some of the figures. The iPad doesn’t have flash but it does a beautiful job rendering PDFs. I have the article in Papers which does an awesome job at holding and organizing my entire medical library.
Basic review of Papers
 Papers is iTunes for scientific Papers. It is the modern equivalent to the file cabinet you always wanted for all the important scientific articles that fall into your grubby little hands. My computer is littered with literally hundreds of scientific articles. What you want to do is throw them all into Papers.
Papers is iTunes for scientific Papers. It is the modern equivalent to the file cabinet you always wanted for all the important scientific articles that fall into your grubby little hands. My computer is littered with literally hundreds of scientific articles. What you want to do is throw them all into Papers.
To understand the power of Papers, let’s look at the workflow for getting a PDF into Papers and onto the iPad. After downloading reference 33, drag it into Papers. It initially looks like this:
On the iPad, when you launch Papers, you are in the Library.
Search on bicarbonate and you find a couple of articles on the use of bicarbonate to prevent contrast nephropathy, one on its use to treat severe metabolic acidosis, and one on its use to prevent the renal complications rhabdomyolysis…bingo!
Papers also works on the iPhone but after using it I thought it was a bit of a gimmick, I didn’t really want my PDF library on a 3.5 inch screen. The iPad makes a perfect partner for the desktop app. I’m very excited about this.
Papers for MacOS is $42.00, the iPhone/iPad application is $14.99.