Every intern knows that the evaluation of hyponatremia includes a TSH and a cortisol level to rule out hypothyroidism and adrenal insufficiency as occult causes of euvolemic hyponatremia.
The mechanism of adrenal insufficiency is a bit confusing with some sources stating that these patients are volume depleted while others are euvolemic.
@askrenal in regards to hypoNa ep w/@kidney_boy a listener wants to know if adrenal insufficiency causes euvolemic or hypovolemic hyponatremia. Apparently various sources disagree. pic.twitter.com/PKsVqq5LVq
— Matthew Watto (@DoctorWatto) April 9, 2018
In some patients without aldosterone, the patients develop severe salt wasting, become hypotensive and get a non-osmotic release of ADH resulting in hyponatremia. These patients will respond to saline. Treat the hypovolemia and the sodium will go up.
Hyponatremia is a common manifestation of adrenal insufficiency even in cases without adrenal crisis. Giving saline to these patients is not effective at correcting the hyponatremia. Giving cortisol, however, results in a brisk water diuresis and rapid correction of the serum sodium (Oelkers, NEJM, 1989).
In addition to being resistant to saline, ADH antagonists (think tolvaptan) protect against this type of adrenal insufficiency-induced hyponatremia.
This means cortisol corrects an abnormality that is due to excess ADH.
Here is the explanation from the late 90’s from The Fluid, Electrolyte and Acid-Base Companion. 
Bartter and Schwartz original definition of SIADH required a normal cortisol specifically to exclude patients with hypopituitism and primary adrenal insufficiency. In primary adrenal insufficiency, in addition to loss of cortisol there is an aldosterone deficiency which can result in sodium wasting, volume depletion and a non-osmotic (decreased perfusion in this case) stimulates for the release of ADH. In this scenario, the patient should appear salt/volume depleted and would not be considered euvolemic.
A nice review of secondary adrenal insufficiency and hyponatremia was done by Sven Diederich.
Remember:
- Primary adrenal insufficiency: destruction of the adrenal glands leads to loss of endogenous cortisol. These patients typically also have aldosterone deficiency, so they will be salt wasters, resulting in hypovolemia. They will also have hyperkalemia.
- Secondary adrenal insufficiency: decreased ACTH (from pituitary or hypothalamic disease, or from pharmacologic steroids) prevents secretion of cortisol
In Diederich’s review they pulled 139 cases of hyponatremia that were referred to endocrinology. (Clearly this study suffers from profound selection bias. Here is a a cleaner study on the epidemiology of hyponatremia by Schrier, from back in the day.) They found 28 cases of hypopituitism leading to hyponatremia. Patients tended to be older (average age 68) and more female (75%). In 25 cases the hypopituitism had not previous been diagnosed and 12 patients had previously been admitted (between 1 and 4 times) for severe hyponatremia without an adequate diagnosis.
Basal cortisol levels were as follows:
- Below 100 nmol/L (3.6 mcg/dL) in 7
- Below 200 nmol/L (7.2 mcg/dL) in 21
- The mean level was 157 nmol/L (5.7 mcg/dL)
- The highest basal level was 439 nmol/L (16 mcg/dL)
Imaging results:
- Twelve patients had an ‘empty sella’
- Six patients had pituitary tumors
-
One had secondary adrenal insufficiency due to chronic treatment with prednisolone because of ankylosing spondylitis
Don’t be the doctor that corrects the hyponatremia but fils to diagnose adrenal insufficiency and discharges and sends the patient home only to redevelop hyponatremia another day. Turn over every stone, especially in patients with SIADH of undetermined etiology.








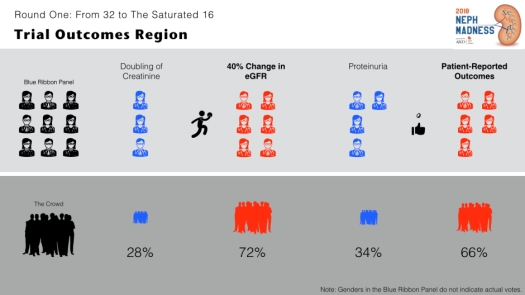






 But in 2018, AJKD forgot to ban gambling. So call your bookie! Mortgage the house! Cash in the kids’ 509 college plan! I’m going to whisper the winners. These darlings are your chance for a better life!
But in 2018, AJKD forgot to ban gambling. So call your bookie! Mortgage the house! Cash in the kids’ 509 college plan! I’m going to whisper the winners. These darlings are your chance for a better life!